The worldwide population is getting older, as people are living longer than ever before. As we age we become more susceptible to certain health conditions, which can reduce our quality of life. This can mean older adults or the elderly can lose their independence and autonomy if they are not able to do things they were before. Osteoporosis, sarcopenia and neurodegenerative diseases are prevalent in the elderly, but if we can look to slow or prevent the deteriorations to the body and mind it can make a huge difference to people living into old age, not just staying alive longer.
Osteoporosis
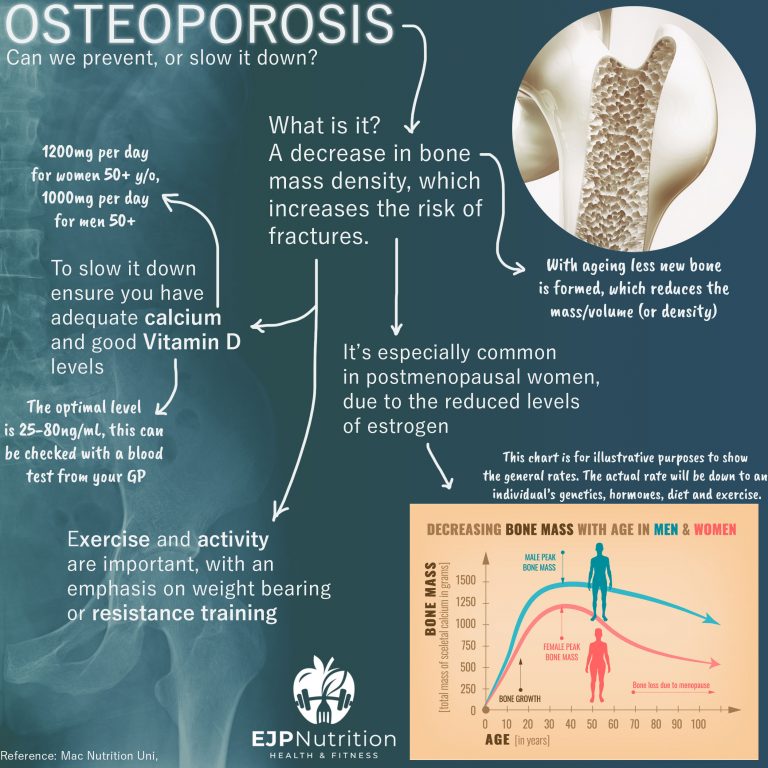
Today let’s start with osteoporosis. This is the weakening of bones, they become more brittle due to a reduction in mass/density and are more susceptible to fractures. Unfortunately there aren’t any symptoms, so unless you’ve had a recent DEXA scan you may not know – until something breaks!
It’s very prevalent in postmenopausal women, as their estrogen levels drop. Estrogen promotes the activity of osteoblasts (which produce bone), so reduced amounts mean there is less new bone being formed. This alongside an increase in osteoclasts (cells responsible for bone resorption, or breakdown) results in weaker bones.
Another risk factor for developing osteoporosis is women who have very low fat levels and who lose their period due to a drop in reproductive hormones (estrogen again!). So anyone dieting to be very lean should be aware of the potential knock-on effects.
Recommendations
So what can we do? One of the causes is a lack of calcium in your diet, so ensure you are getting enough. My calcium post went through how important that is for bone health. For older adults (50+) a higher daily intake of 1000mg for men and 1200mg for women is recommended. Calcium intake is helpful in the prevention and treatment of osteoporosis, so try and get enough in your diet. However if you do struggle, consider a supplement.
Next we’re back to the magic Vitamin D again. This along with fish oil and creatine tend to come up time and again! Vitamin D is closely linked with bone health partly due to it supporting the absorption of calcium. It’s also required for osteoblastogenesis and bone formation. A study found 35%–90% of the institutionalised elderly are estimated to be vitamin D deficient. So correcting some of that could make a massive difference.
For the amount to supplement you’d need a blood test from your doctor for them to advise. Once your levels are in the optimal range, a D3 supplement of 2000-2500IU per day may be beneficial. This depends on where you live, skin colour, how much time is spent outdoors etc.
The last point to note is exercise. Staying active, with an emphasis on resistance training or weight bearing exercise has been shown to be protective. One study noted; Not only osteoanabolic exercises should be recommended; activities aimed to develop muscle strength and body balance and improve the proprioception should be encouraged to prevent falls and fractures.
Starting earlier to stave off the detonation and keep our bones strong and healthy should be a serious consideration. Prevention is better than treatment.
References: Mac Nutrition Uni, Sahni et al 2017, Kennel et al 2010, Demontiero, Vidal & Daque 2012, Matkovic et al 2005, Durosier-Izart et al 2017, Kanis et al 2019, Mangano et al 2019, Duque & Toren 2008, Compher et al 1998, Moriera et al 2014
(Reposted from Instagram)
Bonus Notes:
Some studies have linked dairy or protein intake with increase bone mass density (BMD) too. It’s hard to separate how much was down to the calcium in those diets, or other factors. One study stated; recommendations should include a daily calcium intake of between 800 and 1200 mg and sufficient dietary protein, ideally achieved through dairy products. Another found higher BMD in those with higher dairy intakes, combined with good vitamin D levels.
Another study looked at dairy intake and vitamin D. The higher dairy diet was associated with higher lumbar spine BMD, and protective against trochanter (hip) BMD in vitamin D supplement users compared to nonusers. They concluded; these findings underscore that the benefits of dairy intake on the skeleton may be dependent on vitamin D intake.
I mention these as examples of when we are looking to improve an aspect of our health it’s usually a combination of things that make the difference, rather than one thing in isolation. For osteoporosis for example we have calcium, vitamin D, exercise (RT) then maybe protein/dairy. It again comes back to a balanced varied diet and overall behaviour/lifestyle.